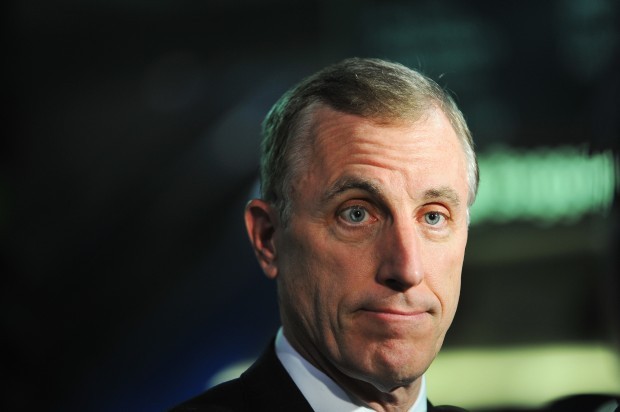
(2-23-17) A tweet by Dr. Jeffrey Lieberman, the chair of the Psychiatry Department at Columbia University, announcing that Miami-Dade Judge Steven Leifman has been appointed as the first Assistant Secretary for Mental Health and Substance Use Disorders is premature. No final decision about the appointment has been made.
“Thrilled with appt. of Judge Steve Leifman as First Asst. Sec. of Mental Health in US History,” Lieberman tweeted.
While Judge Leifman is a strong candidate for taking charge of the Substance Abuse and Mental Health Services Administration (SAMHSA), which has a $3.5 billion budget, Health and Human Services Secretary Tom Price has not officially announced which candidate he will recommend to the White House. The new Assistant Secretary will then have to be vetted and approved – either by President Trump or his staff – before his appointment is sent to the U.S. Senate for confirmation.
For his part, Judge Leifman is not commenting publicly about the tweet or his possible appointment.
Judge Leifman is considered to be the leading candidate because, in my opinion, he is the most qualified and clearly the best choice for the job, a sentiment widely agreed on in Washington.
But he still faces hurdles. When Vice President Mike Pence was governor of Indiana, he appointed Dr. John Wernert to overhaul Indiana’s state mental health system. That could cause problems if Pence decides to get involved. There are still some who are lobbying for a psychiatrist, not a judge, to be put in charge of SAMHSA.
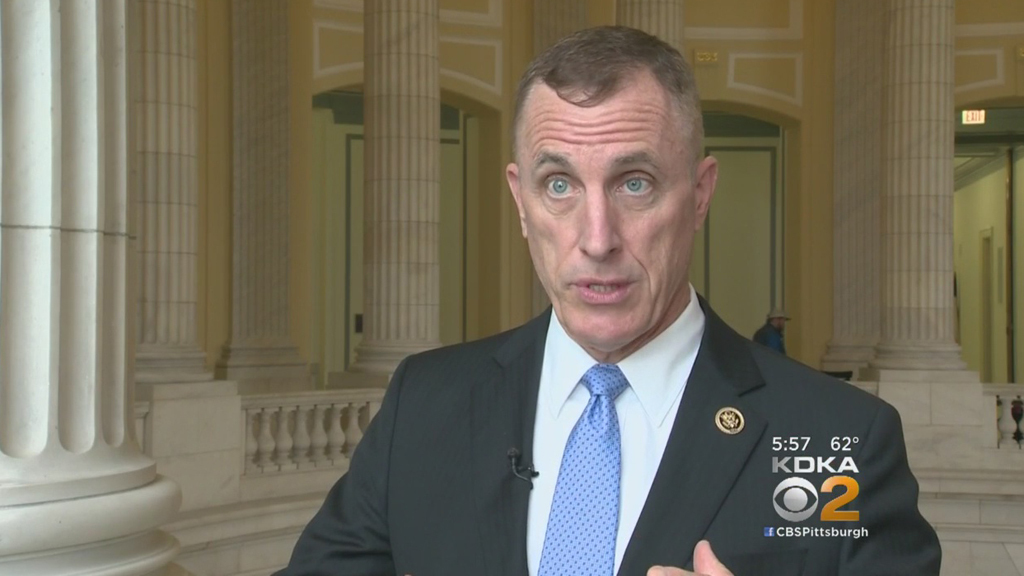
Being a psychiatrist or someone with an equivalent medical background was one of the requirements that Rep. Tim Murphy (R.-Pa.) originally put in his Helping Families in Mental Health Crisis Act (HB- 2646), which started the effort in Congress to reform our mental health system after the Newtown shootings. But that requirement was dropped when Murphy’s bill reached the Senate. Senators didn’t want their hands tied when it came to the confirmation process and they also wondered if a psychiatrist would have the management skills needed to run a large bureaucratic organization.
I have always supported Judge Leifman because I have seen first-hand how he has transformed the mental health care system in Miami-Dade County from one of the most horrific in the nation to one that is now nationally recognized as a “gold standard” model being copied by other progressive communities.
I am not the only one who believes Judge Leifman would be the best choice. Widely admired in mental health circles, Judge Leifman has received strong support from Sen. John Cornyn (R-Tx.) the powerful Senate Majority Whip, and Sen. Bill Cassidy (R.-La.) who co-authored the Senate version of the Helping Families in Mental Health Crisis Act. In addition to his overall knowledge about our mental health system, both were reportedly impressed with his management skills, which are going to be invaluable when it comes to revitalizing SAMHSA. The agency has been blasted by critics, especially Rep. Murphy, and was ranked in a nonpartisan survey by its own employees as one of worst federal agency workplaces.
If you have read my book, CRAZY: A Father’s Search Through America’s Mental Health Madness, you will recall that it was Judge Leifman who got me access into the Miami-Dade County pre-trial detention center so that I could chronicle how jails and prisons have become our new mental asylums. But three years before I knocked on his door, Judge Leifman already had begun working on fixing his community’s badly fractured system. Starting in 2000, Judge Leifman persuaded local stakeholders to sit down, share information and begin cooperating. After my book was published, he got voters to approve a multi-million dollar bond issue to finance alternatives to inappropriate incarceration.
In the past 17 years, Judge Leifman has crisscrossed the nation advocating for jail diversion, Crisis Intervention Team training, mental health courts, and jail intercept and re-entry programs. But he’s wise enough to understand that it takes more than keeping ill individuals out of our criminal justice system to help them regain control of their lives. He serves on the board of the nation’s largest and most successful supportive housing organization, is on the board of the American Psychiatric Foundation, and is an enthusiast of job training, clubhouses, peer support services, and imaginative recovery programs.
Under his leadership, Miami-Dade County has become the first in the nation to investigate how predictive analytics can be applied to mental health and substance abuse services. In addition to working locally, he was appointed a Special Advisor on Criminal Justice and Mental Health for the Supreme Court of Florida. On November 19, 2015, he became the first Floridian judge to receive the William H. Rehnquist Award for Judicial Excellence from U.S. Supreme Court Chief Justice John Roberts – the highest honor that a judge can receive from his peers.
Because judges in Florida are non-partisan, Judge Leifman was able to get both Democrats and Republicans in the state legislature during its last session to pass the most sweeping mental health legislation in the state’s recent history. Hopefully, his ability to work with both parties will help him if he is named and has to undergo Senate confirmation.
Let’s hope that Dr. Lieberman’s premature tweet eventually becomes reality because Judge Leifman is exactly the right leader for the Assistant Secretary job and our best hope for true reform.
The post Tweet Declaring Judge Leifman As Our New Mental Health Czar Is Premature. But Let’s Pray That He Is Selected appeared first on Pete Earley.